How to Address Oral Candidiasis in Immunocompromised Patients
Posted on August 06, 2024 by Admin
How to Address Oral Candidiasis in Immunocompromised Patients
Oral candidiasis is the more common name of a disease that is a fungus that is caused by Candida species, mainly Candida albicans. One of the issues that are liable to be more troublesome for immunocompromised patients than otherwise healthy individuals is the weakened defense of the immune system. Dealing with oral candidiasis in individuals like that is a threefold process, i.e. correct and early recognition of the disease, right diagnosis of the disease, and effective treatment.
Understanding Oral Candidiasis
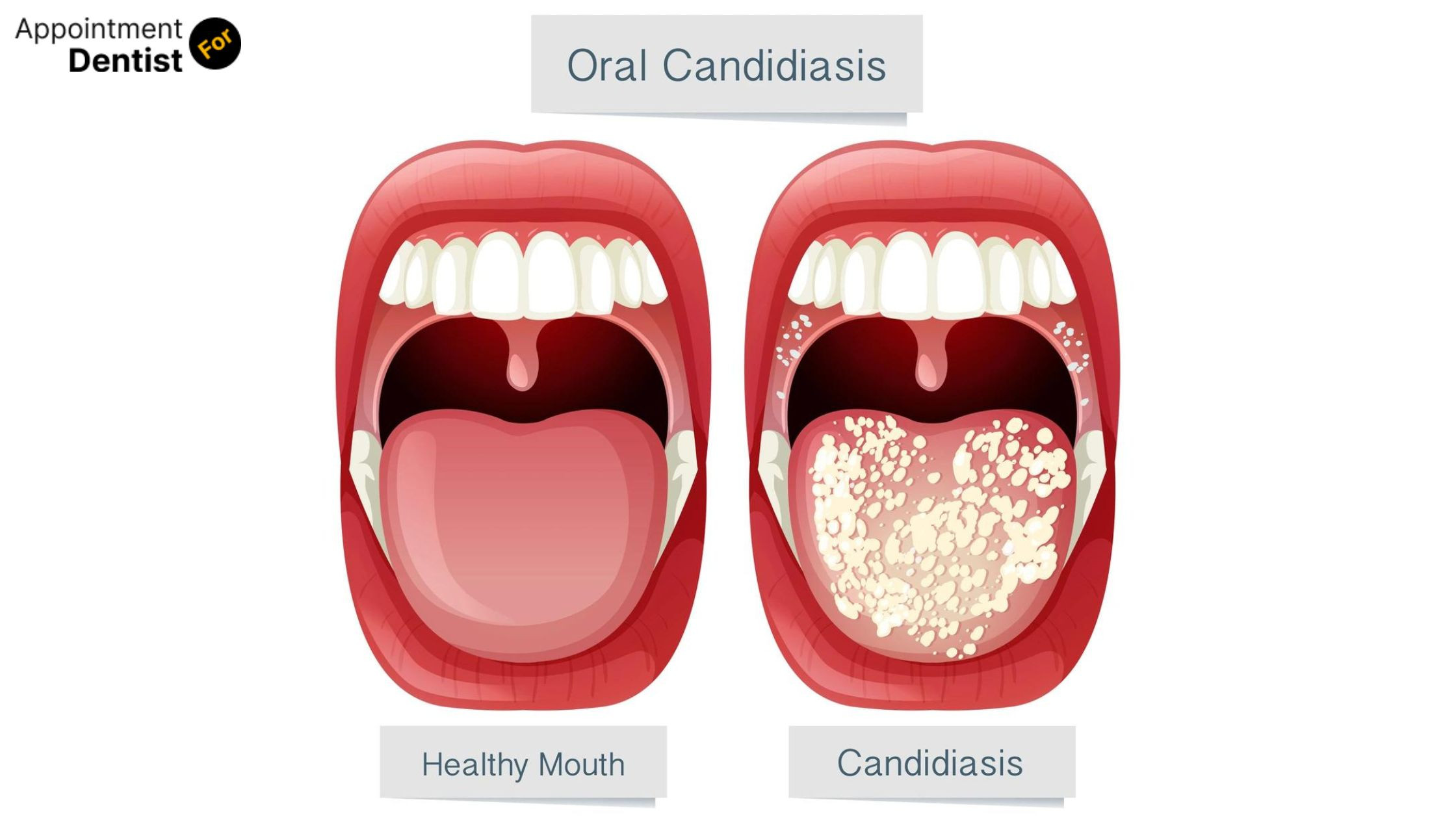
Oral candidiasis presents as white leucoderma raised areas on the oral mucosa that is frequently accompanied by redness, painful tongue problem, and impaired swallowing. In case of immunocompromised patients, these abnormalities may become more complex and unabated, thus, may give rise to the danger of systemic infections if no cure is applied.
Immunocompromised, such as chemotherapy patients, those with HIV/AIDS, organ transplant recipients, or individuals on long-term corticosteroid therapy, are especially prone to oral candidiasis.
Recognizing the Symptoms
Seeing it early is a good way to keep it in control. Symptoms that you can watch out for are:
- White Patches: Among the specific areas are the tongue, inner cheeks, gums, or the roof of the mouth. Those may appear as lumpy things similar to cottage cheese and can be wiped away while the red spots and, thereby, the swollen areas beneath being uncovered.
- Redness and Soreness: It may not always be that irritation is localized over regions in the presence of paleness, thus giving rise to discomfort during food consumption and swallowing.
- Difficulty Swallowing: This can happen if the infection is transferred to the throat or esophagus, which, actually, makes the problem more complicated.
- Loss of Taste: Quite a number of patients are likely to experience flavors’ perceptions changes in the somatic cells or may be manifested through a number of modalities as an unpleasant taste.
Diagnostic Approaches
A proper diagnosis of a fungus in the oral cavity can be done via both physical examination and laboratory tests:
- Clinical Examination: A physician will diagnose the typical white lesions and other symptoms that are characteristic of the disease. The correct identification of the disease in immunocompromised patients is the doctor's work which is why it is necessary to establish whether this is a candidiasis or an infection.
- Microscopic Examination: Lesion scrapings from the oral cavity are collected for examination at the microscopic level to identify the Candida species.
- Culture: Oral lesions may be subject to a mouthwash and the sample then undergoes culture in the lab where it will be tested for Candida and also for specific strain determination.
- Endoscopy: When there is a possibility of the infection being spread to the esophagus, an endoscopic examination of the upper digestive tract may be advised.

Also Read: Things You Should Know About Dental Insurance
Management Strategies
-
Antifungal Medications
The use of antifungal medicines is the number one means of treatment for oral candidiasis. The medication choices and the treatment location according to the severity of the disease and the health state of the patient must be made by the therapist.
- Topical Antifungals: These drugs including Nystatin and Clotrimazole are first-line treatments for mild or moderate instances. They are applied in combination as lozenges or by suspensions and their efficacy has been observed for conditions that are mild which are the common ones affected.
- Systemic Antifungals: Systemic antifungals with the likes of fluconazole or itraconazole can be given to patients who have severe cases that are not responding to antifungal medications themselves. These are usually taken by mouth or through a vein and they are primarily applied for prolonged infections or if the local therapies are ineffective.
-
Addressing Underlying Conditions
For immunocompromised patients, managing the underlying condition is crucial to prevent recurrence. This might include:
- Optimizing Immunosuppressive Therapy: To the patients undergoing any form related drugs, it may be commended to adjust the dosage or consider switching to weaker immunosuppressive ok*with them while consulting their doctor on the options.
- Diabetes Control: Among the diabetic patients, it has been found that efforts to catch on with controlling the glucose level can lower the risk of obtaining fungal infections.
-
Maintaining Oral Hygiene
Oral hygiene is of paramount importance to manage and prevent oral candidiasis and the following are some of the practices that can be followed:
- Regular Brushing and Flossing: Patients have been advised to brush their teeth twice a day and regularly floss so that they could get rid of the food particles that are deposited there and also the plaque.
- Rinsing with Antifungal Mouthwash: An antifungal mouthwash is prescribed which can also be a remedy by its use.
- Avoiding Irritants: Patients have to quit using tobacco, not to drink alcohol, and do not need to use the ones with alcohol content in them, as these can irritate the oral mucosa and exacerbate symptoms.
-
Dietary Considerations
Diet is among the very important means in handling oral candidiasis:
- Reducing Sugar Intake: Candida prospers in the zone where there is an excess of sugar, therefore, through sugar and refined carbohydrates intake, it is possible to inhibit the growth of the fungi.
- Eating Yogurt: As per some of the research conducted, yogurt with live cultures may assist in the maintenance of proper oral flora.
-
Patient Education and Follow-Up
Informing people about their situation and impressing upon them the necessity for consideration towards a treatment schedule are fundamental rights. It has been prescribed for patients that after some time they can see their doctors in a regular manner, so that, on the one hand, doctors have a possibility to evaluate common signs and adjust treatment accordingly on the other patients get earlier help if needed.
Also Read: The Connection Between Diabetes and Oral Health: Managing Gum Disease
Preventing Recurrence
Avoiding of the repeated occurrence of oral candidiasis among the immunocompromised patients can be the aim of the following techniques:
- Routine Screening: Standard practice of regular oral examinations to detect early onset of the infection.
- Continued Antifungal Prophylaxis: Prophylactic treatment with antifungals may be recommended for high-risk patients, so that they can avoid having the infection again.
- Regular Monitoring of Immunosuppressive Therapy: The option of altering drugs based on immune status and general health may be used to prevent the occurrence of infections.
Conclusion
Oral candidiasis in immunocompromised patients should be managed rapidly and adequately with the aim to avoid complications and improve life quality. By diagnosing the symptoms early and using proper diagnostic methods, as well as employing treatment strategies, the healthcare providers can help decrease the impact of this fungal infection. The continuous teaching and regular follow-up of patients are key elements for successful management and prevention of recurrence. With a shared decision-making and treatment compliance, patients can effectively deal with their oral candidiasis and overall maintain good health.
Faqs
-
1. What is oral candidiasis?
Oral candidiasis, or oral thrush, is a fungal infection in the mouth caused by Candida species, typically Candida albicans. It appears as white patches on the tongue, inner cheeks, or other areas in the mouth and can cause soreness and difficulty swallowing.
-
2. Why are immunocompromised patients more susceptible to oral candidiasis?
Immunocompromised patients, such as those with HIV/AIDS, undergoing chemotherapy, or on long-term corticosteroids, have weakened immune systems that struggle to control fungal overgrowth, making them more prone to infections like oral candidiasis.
-
3. How is oral candidiasis diagnosed?
Diagnosis involves a clinical examination of oral lesions. Confirmatory tests may include microscopic examination of a lesion sample, culture to identify the Candida species, and endoscopy if the infection is suspected to extend beyond the mouth.
-
4. What are the primary treatments for oral candidiasis?
Treatment typically involves antifungal medications. Mild cases may be treated with topical antifungals like nystatin or clotrimazole, while severe cases might require systemic antifungals like fluconazole or itraconazole. Addressing underlying health conditions and improving oral hygiene are also crucial.
-
5. How can oral candidiasis be prevented in immunocompromised patients?
Preventive measures include maintaining good oral hygiene, managing underlying health conditions, reducing sugar intake, and possibly using antifungal mouthwash or prophylactic antifungal treatments as recommended by a healthcare provider. Regular follow-ups and monitoring are also important.
Recent Post
- The Importance of Oral Health Education for Children
- How to Choose the Right Orthodontic Treatment for Adults
- The Link Between Oral Health and Stroke Risk
- How to Address and Prevent Gum Recession
- Innovations in Dental Anesthesia: Pain-Free Procedures
- The Role of Saliva in Oral Health: Functions and Disorders
- Exploring Holistic Dentistry: What You Need to Know
- How Oral Health Affects Your Immune System
- The Benefits of Using Dental Probiotics
- Oral Health and Pregnancy: Myths and Facts